
UNC School of Medicine
The UNC School of Medicine and Department of Pathology and Laboratory Medicine are housed within this structure. The three coequal missions of the UNC Department of Pathology and Laboratory Medicine are
Indiana University School of Medicine
The IU Simon Cancer Center houses more than 200 scientists and conducts research from four different programs. The goals of those programs range from understanding the molecular changes that cause cancer to
Purdue University
Purdue University is home to a nationally and internationally ranked School of Mechanical Engineering and NCI-designated Purdue Center for Cancer Research. Consistently highly ranked, the School of Mechanical Engineering has been at the forefront of providing the most respected engineering research and education in the world. Seventy-four faculty members are dedicated to educating over 1,800 undergraduate, graduate students and postdocs, and to maintaining and developing world-class research programs.

Matthew J. Flick, Ph.D.

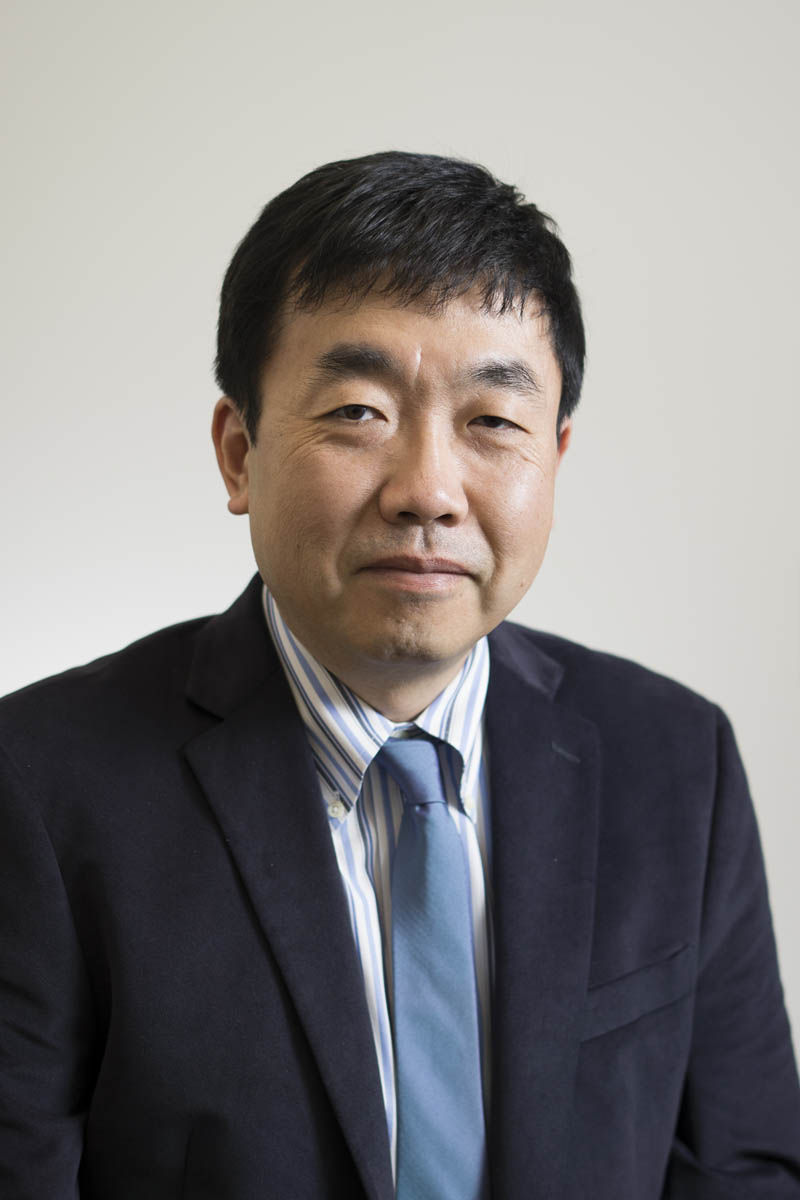
Melissa Fishel, Ph.D.
Bumsoo Han, Ph.D.


Alisa Wolberg, Ph.D.
Specific Aims of the UNC School of Medicine Program
The fundamental connection between coagulation system dysregulation and malignancy has been recognized for over 150 years. A prime example of this connection is pancreatic ductal adenocarcinoma (PDAC), which has the highest risk of cancer-associated thrombosis and has one of the highest mortality rates of all cancers. PDAC will soon be the second leading cause of cancer deaths in the U.S. with a 5-year survival rate of only 7%, a number that drops to 2% for individuals with metastatic disease. Poor survival is linked to the aggressive and invasive nature of the malignancy and the frequency of associated devastating thrombotic events. A more thorough understanding of the functional pathways will provide a unique opportunity to limit both progression of the cancer and thrombotic complications.
The prothrombotic potential of PDAC has been directly linked to high-level expression of Tissue Factor (TF) by PDAC tumor cells that drives exuberant thrombin activity in circulation and in the tumor microenvironment (TME). In the TME, thrombin activates the G-protein coupled protease activated receptor-1 (PAR-1) on target cells, including PDAC tumor cells and stromal cancer-associated fibroblasts (CAFs). Our preliminary data suggests that PAR-1 signaling by PDAC and CAFs leads to production of the plasminogen activation (PA) system components urokinase plasminogen activator (uPA) and receptor (uPAR) that play critical roles both in the TME to drive PDAC tumor progression and in the thrombotic potential of the developing malignancy. The long-term goal of this program is to fill crucial knowledge gaps by defining the bi-directional mechanisms through which the PAR-1/PA axis (i) accelerates PDAC tumor growth, invasion, and dissemination and (ii) simultaneously enhances TF-driven thrombosis in PDAC disease. Through the CLOT research program, our project will pursue three specific aims:
Aim 1, Determine how PAR-1 mediates uPA and uPAR-driven PDAC tumor progression that exacerbates thrombosis in vivo. PAR-1 is highly expressed by PDAC tumor cells and our preliminary data strongly suggest that PAR-1 signaling drives uPA and uPAR expression in these same tumor cells. Our hypothesis is that PAR-1 activity in KRASG12D/TP53R172H tumor cells and CAFs supports PDAC progression through induction of uPA and uPAR, and in so doing drives PDAC-associated thrombosis. The scientific premise of these studies builds on established observations to provide a definitive mechanistic analysis of how PAR-1 and uPA activity influences both PDAC progression and the PDAC-associated prothrombotic activity. Our approach is to employ cell type-specific knockouts together with de novo and transplantable KPC-mediated PDAC models to define the role and mechanistic underpinnings of the PAR-1:uPA axis.
Principle Investigators: Matthew Flick and Alisa Wolberg
Aim 2, Define the cell specific mechanisms of tumor cell- and CAF-derived PAR-1 and uPA/uPAR function in mediating tumor cell proliferation/invasion. A hallmark of PDAC is the ability of this malignancy to locally invade tissues and remodel the extracellular matrix to promote growth and ultimately metastasis. We hypothesize that a major factor driving this ability is PAR-1 activity leading to induction of uPA and uPAR in (i) KRASG12D/TP53R172H epithelial cells to promote tumor cell invasion and release of prothrombotic potential (i.e., tumor derived TF+ microvesicles) and (ii) CAFs to establish and organize a highly desmoplastic TME. The scientific premise of this Aim is based on observations indicating that the degree of fibrosis in PDAC is driven in part by PAR-1, it correlates with a poor prognosis, and is a factor driving chemoresistance. Our approach is to employ a novel biomimetic 3D tumor model system that reconstructs the PDAC TME to elucidate cell- and process-specific mechanisms by which PAR-1/PA drive PDAC progression and enhance prothrombotic potential.
Principle Investigator: Bumsoo Han
Aim 3, Investigate the link between uPA/uPAR expression in patient tumors and the efficacy of antifibrinolytic therapies to both limit PDAC progression and, paradoxically, suppress thrombotic potential in a patient-derived xenograft model. PDAC typically is diagnosed at advanced stages of disease, where chemotherapy is marginally effective and the occurrence of VTE most prominent. Our hypothesis is that pharmacological reduction of plasminogen or plasminogen activation system components will limit the growth of even advanced human PDAC tumors and the ability of these tumors to drive thrombosis. As an essential proof-of-concept, we will determine if pharmacological elimination of plasminogen or suppression plasminogen activity are effective in limiting tumor growth and cancer-associated thrombosis in clinically relevant in vivo models. The scientific premise is based on (i) findings that high tumor expression of uPA and high circulating D-dimer significantly correlates with poor patient survival; and (ii) our preliminary studies indicating that tumor cell expression of uPA and uPAR, as well as circulating plasminogen, promote PDAC progression. Our approach is to utilize characterized low passage patient-derived tumor and CAF lines as well as PDAC patient tumor tissue to determine whether expression of uPA and uPAR are linked to aggressive growth and exacerbation of venous thrombosis in patient-derived orthotopic xenograft models.
Principle Investigators: Melissa Fishel and Alisa Wolberg
